WASH and COVID-19: some notes for interventions
Data collected and elaborated by Giorgio Cancelliere, Giuseppe Bolzoni and Stefano Gambini, on 1st of June 2020
Here are some notes and suggestions regarding the WASH sector in the prevention of COVID 19. The notes were collected with a group of colleagues who collaborate with the Italian Civil Protection and the Italian Red Cross, and represent training material to be integrated with the already widespread practices and materials on hygiene and the WASH sector in general. Recent WHO publications are being published to deal with the COVID-19 emergency.
These notes do not claim to be exhaustive neither on how to carry out COVID-19-related interventions nor to give the completeness of the actions to be implemented out; they aim to give a quick reference on the actions to take when we want to address an anti-COVID-19 campaign in the countries where we intervene.
The main objective of WASH interventions in emergency and in general is to reduce the transmission of faecal-oral diseases and the exposure of vectors that transmit diseases, through the promotion of good hygiene practices, the distribution of good quality water and the reduction of health risks in the environment. As for the transmission of viruses, the main exhaustive guidelines are those of the WHO, which mainly regard the quality of the water, the sanitation standards and the treatment and disposal of sanitary materials used during the epidemic (pandemic). Any barrier that can be raised to prevent pathogen faecal-oral or respiratory droplets transmission, is important in planning the fight against the virus.
The indications collected here should support NGO's interventions at health centers, hospitals and dispensaries where the virus is more easily transmitted as the first reference places of sick people, schools, bus stations, markets and railway, river or sea boat stations. The request for first assistance and people aggregation are important vectors for the dissemination of the virus.
Barriers to prevent contamination
What we known about COVD-19 refers to past experience in dealing with viruses of the same type (in particular enveloped RNA coronaviruses, similar in both morphology and structure) and some influenza viruses. It is worth noting that for COVID-SARS viruses no vaccine has been produced and the only actions to prevent the spreading are isolation (distancing)n and hygiene. Unlike SARS, however, COVID-19 has a much longer latency period preventing the outbreak of infection with the manifestation of symptoms, causing a large number of asymptomatic patients. This situation, therefore, requires widespread preventive actions that involve both health facilities and the community as a whole. Widespread preventive actions include all the hygiene practices that we regularly use in hygiene and sanitation projects and now they must be delivered for the prevention of COVID-19.
The virus COVID-19 is transmitted through air particles or direct contact with infected person and/or infected surfaces. Another important mean of transmission is through the use of hands (direct contact). On average, we touch our face 23 times in an hour, allowing the virus to pass through the wet surfaces of our mouth, nose and eyes. This type of transmission is the least "perceived" as we do not realise the many times we use our hands in daily life.
Traces of COVID-19 have been found in the feces of infected people since COVID-19 affects not only the lungs but, among other organs, also the intestines. A percentage ranging from 2% to 27% of infected cases had diarrhea, with COVID-19 RNA residues in fragments of the faeces. Like most enveloped RNA viruses (capsid: protein envelope), their fragments do not last longer than 2 days in a sewer system before disappearing.
Although the spreading of the virus through faeces and their disposal have not been fully verified, preventive practices are nonetheless strongly recommended because the contact with the virus can be cause of immediate infection, due to its cellular devastation action. Enveloped viruses are more stable in the environment than non-enveloped viruses.
The following conditions help to reduce the survival of viruses:
- High temperatures
- Sunlight exposure
- Low or high pH
Preventive remedial
Based on the SARS-CoV-1 experience, the virus can remain on the surface for 2 hours to 9 days, depending on the type of surface, temperature, humidity and strain of the virus. The use of appropriate disinfectants, such as a solution to 70% ethanol or 0.1% sodium hypochlorite (commonly found on the market at 5% Chlorine – Bleach), can reduce the exposure of the virus to 1 minute. Hypochlorite is quickly inactivated in the presence of organic material. Therefore, regardless of the concentration used, before applying the solution it is important to thoroughly clean surfaces with soap and water or detergents through mechanical actions such as scrubbing. For this reason, it is recommended to regularly clean all surfaces that can be infected. Never mix detergents with active chlorine solutions.
To prepare a sanitizing product at home (for home surfaces), we recommend following the instructions from the WHO here.
Components can be found in the pharmacy or at the supermarket. Below are the doses to prepare 500 ml of disinfectant:
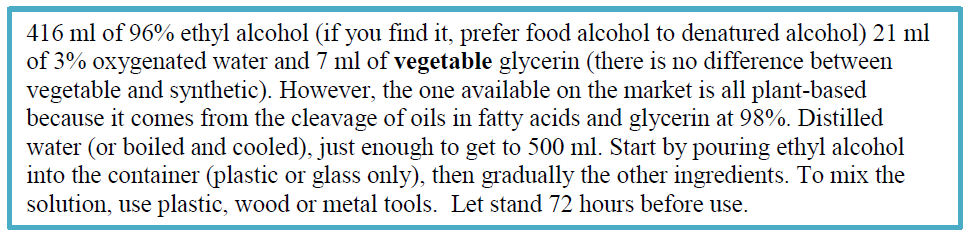
To prevent evaporation of WHO disinfectant solution (estimated price: 0,37 USD/100 ml), containers should have a maximum capacity of 500 ml on ward and 1litre in operating theatres, and ideally fit into a wall dispenser. Leakage-free pocket bottles with a capacity of no more than 100 ml should also be available and distributed individually to health-care workers, but it should be emphasized that the use of these products should be confined to health care only. Plastic bottles can be recycled.
In health facilities, the WHO recommends using:
- 70% ethyl alcohol to disinfect small surface areas and equipment between uses, such as reusable dedicated equipment (for example, thermometers);
- sodium hypochlorite at 0.1% (1000 ppm) for disinfecting surfaces and 0.5% (5000 ppm) for disinfection of blood or bodily fluids spills.
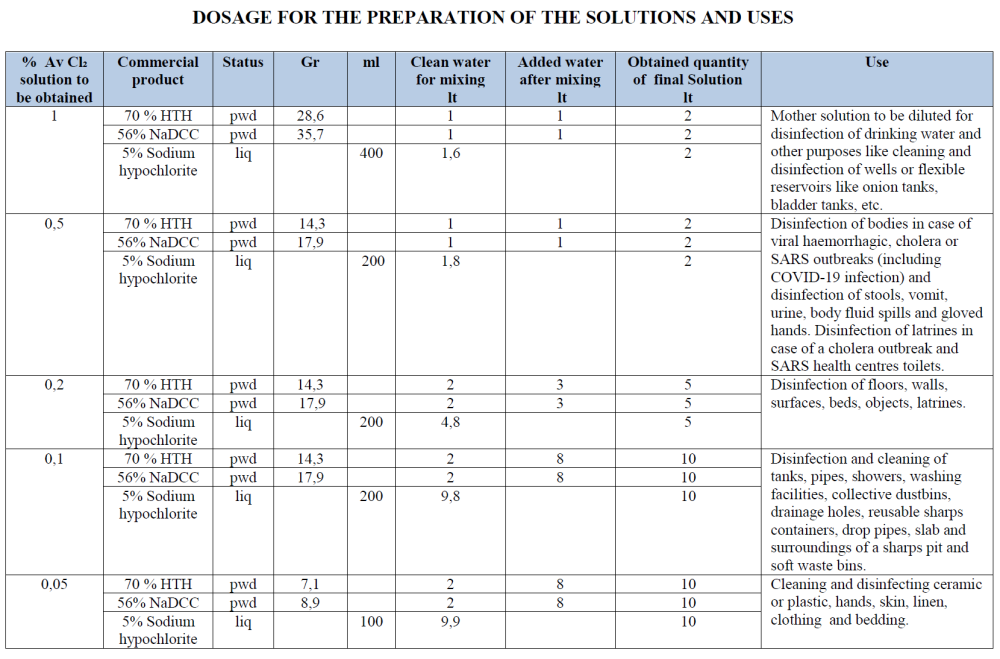
Active Chlorine (AvCl2) in various concentrations is widely used as a disinfectant. Below is a guide for the preparation of products at different concentrations of AvCl2, according to its final use: hands, floors, surfaces, toilets and other objects. Never use Chlorine products on roads, sidewalks, courtyards, etc. Chlorine is immediately degraded by light and the mineral and organic substances present. Outdoors, it is necessary or sufficient, to clean surfaces with water and detergent.
Guide on how to prepare a chlorine solution
It necessary to operate in a ventilated space, wear a pair of gloves, a pair of goggles, a mask and protecting clothing like a plastic apron to protect skin. Some tools like plastic buckets and plastic spoons are necessary. Never use metallic tools.
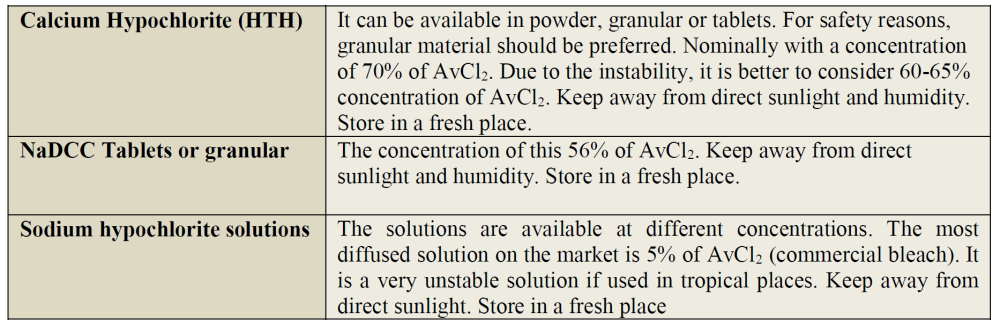
It can be used a product able to release active chlorine. It can be in powder or in solution. The products available on the market are:
DOSAGE FOR THE PREPARATION OF THE SOLUTIONS AND USES
To calculate Active Chlorine solutions, we recommend the use of Chlorine Management App, a mobile application developed by the Water and Habitat Dpt of ICRC in response to the Covid-19 pandemic. The application is ideally suited for those working in (limited-resource) health care settings and allows users to easily identify the recommended protocol for disinfection.
Apple: https://lnkd.in/dziCXei
Android: https://lnkd.in/djNhTKd
General indications for handling AvCl2 solutions
Use plastic bucket. Always wear protective tools when used. Store the solution in a fresh place for not longer than 4 days and not exposed to sunlight and to high temperature. The efficiency of the solution will rapidly diminish, as shown in the graph (concentration, time and temperature). Solutions at lower concentrations of chlorine decompose slower. In the case of commercial bleach (5% AvCl) the three curves are much flatter and the product is more stable. It is advisable to make packages of limited volume, regenerating them often.
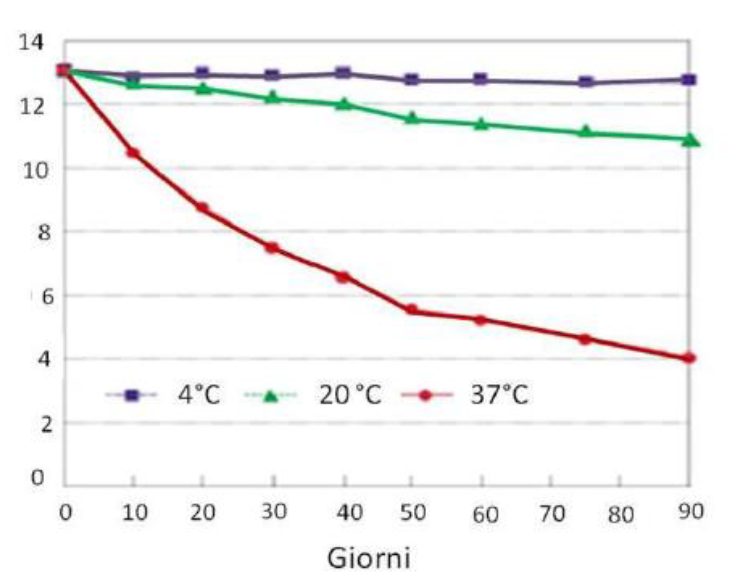
Chlorine solutions easily decompose based on:
1. The concentration of hypochlorite;
2. The pH of the solution;
3. The temperature of the solution;
4. The concentration of impurities that catalyze decomposition;
5. The exposure to light.
Close attention should be applied during transport since hypochlorite easily degrades. For sodium hypochlorite, it is not recommended to carry it beyond 200 km, possibly in solution lower than 5% of AvCl2 and keep it in a cool place (wrap it in wet rags), away from direct light and check that there is no bulge in plastic bottles. For the calcium hypochlorite in granules (70% AvCl2), it must be transported in special containers (25 Kg for air transport and 45 kg for road and sea transport) as it can generate toxic gases and also explosive mixtures in presence of moisture. Always store it in cool places.
Frequency of disinfection.
a.- Hospital wards: 3 times per day
b.- Office floors and surfaces: Once a day
c.- Toilets: Twice a day.
Hand washing soap
Handwashing is recommended after coughing and sneezing and/or disposing of a tissue, on entering the home having come from public places, before preparing food, before and after eating and feeding/breastfeeding, after using the toilet or changing a child’s diaper and after touching animals.
Handwashing with soap is identified as one of the most critical actions for preventing the spread of COVID-19. Proper handwashing is not a guarantee to always protect against COVID-19, but it is an immediately available and affordable method to help protect yourself and others and reduce its spread. Soap does not need to be liquid or anti-bacterial; any regular bar of soap is effective. Contrary to popular belief, regular soap is just as effective as alcohol-based hand sanitizer.
In case washing hands with soap is not possible or while performing sanitary interventions we recommend a solution of alcohol (about 70% ethanol alcohol). In this case, the amount of alcoholic solution to use is the one necessary to maintain your hands completely wet.
For proper cleaning of hands, it is recommended to scrub them with soap for 20-40 seconds if the water is of good quality, for 40-60 seconds if the water is of poor quality and partially contaminated (muddy water with less than 10 families of faecal coliforms). The quality of the water used for handwashing does not have to meet drinking water standards. Reported amounts of water used for handwashing that diminishes faecal contamination range from 0.5 to 2 litres per person.
When we touch a contaminated surface, the virus moves onto our hands, sticking to the fat that covers it. The surfactants present in soaps and detergents have two main functions:
- they take away the fat and dirt on the skin and remove also the virus;
- they act on the virus and disrupt its structure.
The surfactants hook these fats and eliminate them by disrupting their envelope. These are the reasons why the World Health Organization highlights the use of soaps as one of the most effective actions to mitigate the effects of the epidemic: it will not make it disappear overnight, but it will certainly make the life of the virus more difficult. However, when making soaps to prevent the spread of the virus attention must be paid to the presence of surfactants. Most surfactants are chemical, therefore their contact with the skin should be limited.
There are many methods to produce soap, and they are easily accessible on the internet. As an action against coronavirus, we recommend alkaline soaps (basic). Alkaline soaps can be produced by adding ash. Ash itself could represent the last-resort alternative for hand washing but it should be highlighted that it is very aggressive for the skin. Ash can kill viruses because it forms an alkaline solution when mixed with water.
The wood ash consists mainly of calcium carbonate, between 25% and 40%. Potassium carbonate is around 10% and less than 1% phosphate, but there are other elements. Calcium carbonate is insoluble in water so it has no impact on alkalinity. Potassium carbonate is soluble and determines the pH of the watery solution in which the ash is dispersed (the final pH is around 10, which is strongly alkaline for the skin). Ash can also be mixed with sodium bicarbonate (baking soda at pH 8), which decreases the level of alkalinity, to make a bar of homemade soap alternative. In order to lower the high pH and aggressiveness of the ash, add a sour solution (vinegar or lemon juice) to the still melted finished soap and mix.
For handcrafted soap production, see here
To optimize the use of soap in bars, place dispensers in areas of strong passage. See for example: http://www.xopi.org/.
Steps to take for a COVID-19 protection intervention
The key part of any intervention is to understand the degree of learning that the population has of the virus, the damage it can do, how it spreads and the practices to be adopted to lower the risk of contamination. At this stage, in addition to a direct sample survey of the population, all the information tools of the health authorities must be collected and validated to verify the exact approach and to coordinate in the best way in the prevention action.
- Identify the health care centers and ensure that health workers have the proper protection to intervene (masks, gloves, glasses, disposable suits, shoes). Check the availability of basic drugs.
- Identify, together with local institutions and population, the most accessible points for gatherings, estimating how much population accesses it and how often. If possible, make a map with density estimation and opening hours for schools, markets, dispensaries, health centers, etc. Estimate that in the event of an epidemic the consumption of water to wash hands can be as high as 2 l/d/person.
- Identify all influencers who can increase the dissemination of messages to be promoted and select the people who can manage the distribution points of disinfectant products, ensuring quality, continuity and accountability.
- Create a database for each distribution center with the following information:
- Name;
- GPS location;
- Institutional or Community Manager of the Centre or NGO/CBO;
- Reference person (ID, mobile phone number);
- Amount of people/hours present;
- Opening time;
- Sales personnel, services for the supply of masks, gloves and sanitizing materials.
Interventions to be performed:
- Disinfecting using appropriate material and quantity of water: water (l/p/g), disinfectant (grCl/p/g or gr/soap/person/day), paper to dry hands. For the personnel in contact with COVID-19 patients, it is recommended to wash hands at least once per hour.
- Construction of protective barriers or structural interventions to ensure distance and separation (assisted paths, Plexiglas, division of outlets, etc.). For surface disinfection, it is recommended that you use data reported above and consult this site
- Latrine construction, improvement and sanitation. For more details, visit this site
- Deploy low-cost hand-washing systems. For more details, please visit here.
For interventions in health centres, please refer to the guidelines prepared by UNICEF/WHO.
To schedule a WASH intervention and a campaign on COVID-19, we recommend that you consult this text, which also includes data collection cards
To plan and estimate a budget to address a COVID-19 intervention, we recommend that you consult the WHO COVID-19 Essential Supplies Forecasting Tool (COVID-19 ESFT)